Introduction
The gastrointestinal tract is the most common extranodal site involved in non-Hodgkin lymphoma (NHL) and most NHL cases are of B-cell origin. Peripheral T-cell lymphoma (PTCLs) involving the gastrointestinal is less commont, comprising only about 4-6% of gastrointestinal lymphomas. This study retrospectively analyzed the clinical characteristics and potential clinical factors influencing survival outcomes in patients diagnosed with PTCLs through gastrointestinal tissue biopsy at our center.
Methods
Based on the clinical data, patients were reevaluated for clinical staging and risk stratification, including Ann Arbor staging, IPI scoring, and gastrointestinal lymphoma Lugano staging. Patient's follow-up was conducted through outpatient medical records and telephone communication.
For the analysis of categorical data, the chi-square test or Fisher's exact test was used. Survival time was estimated using the Kaplan-Meier method. The Cox proportional hazards model was employed to calculate hazard ratios (HR) and their 95% confidence intervals (CI) to analyze prognostic factors. Data analysis was performed using SPSS 23 for Windows software.
Results
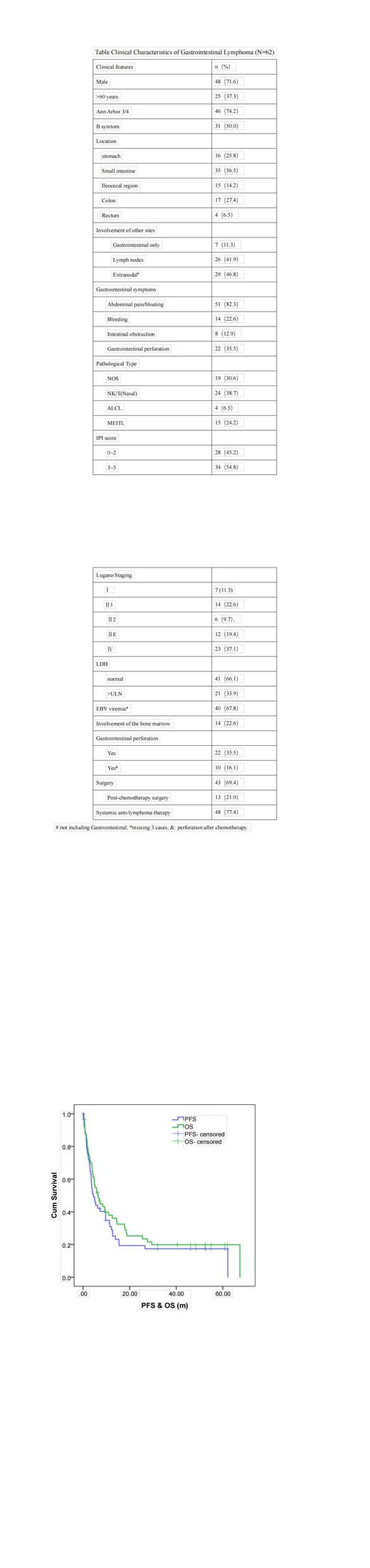
A total of 622 gastrointestinal tissue biopsy samples from October 2014 to September 2022 were retrieved from the medical records system. Among them, 67 cases (10.8%) were diagnosed as PTCLs. Among them, 5 cases had no available clinical data and were excluded. Detailed information regarding patient clinical characteristics can be found in the table.
Treatment and Efficacy:
Among the 62 patients with available clinical data, 43 received gastrointestinal surgical resection treatment, including 21 cases (33.9%) of elective non-emergency surgery and 22 cases (35.5%) of emergency surgery due to acute abdomen. The median courses of chemotheray was 5 (1~8). 15 patients (31.3%) achieved complete response (CR)/CRu; 10 patients (20.8%) achieved partial response (PR).
Among the 59 patients who received chemotherapy and/or surgical treatment, progression-free survival (PFS) was evaluated with a median follow-up time of 48.4 months, and the median PFS was 4.4 months (95% CI: 2.5-6.3) (Figure). Multivariate analysis identified advanced Ann Arbor stage (stage 3/4) (HR=3.53, 95% CI: 1.53-8.17, P=0.003) as independent adverse prognostic factors for PFS. Receiving chemotherapy (HR=0.24, 95% CI: 0.09-0.66, P=0.005) and elective surgery (HR=0.45, 95% CI: 0.22-0.92, P=0.029) were identified as independent favorable prognostic factors for PFS.
As of the last follow-up, a total of 49 patients (79.0%) had died and the median overall survival (OS) was 6.4 months (95% CI: 3.8-8.9) (Figure). Multivariate analysis identified Ann Arbor stages 3-4 (HR=3.01, 95% CI: 1.34-6.74, P=0.007) as an independent adverse prognostic factor for OS, and receiving chemotherapy (HR=0.13, 95% CI: 0.05-0.31, P<0.001), elective surgery (HR=0.36, 95% CI: 0.16-0.74, P=0.006) were identified as independent favorable prognostic factors for OS.
Conclusion
Data from four hematological disease treatment centers located in Zhejiang Province, southeastern China, showed that PTCLs involving the gastrointestinal tract accounted for approximately 10.8% (67/622) of all gastrointestinal lymphoma patients. These patients had a relatively high incidence of gastrointestinal perforation (35.5%). The overall treatment efficacy for patients was poor, with a majority of them succumbing to disease progression. The median PFS and OS were approximately six months. Elective surgery and chemotherapy appeared to improve the patients' outcomes.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal